Dr. Daisy Chemaly & Associates
Oral and Maxillofacial surgery and pathology
305 South Kingsway Toronto, Ontario M6S 3V5 Phone: 416-766-7616 Fax: 416-766-7617
Procedures & Services
- 2D & 3D IMAGING
- All About Wisdom Teeth
- What is an impacted tooth?
- Dental Extractions
- Bone Grafting And Reconstruction
- Dental Implants
- Guided Implant Surgery
- Oral Pathology
- TMJ (Temporomandibular Joint)
- Corrective Jaw (Orthognathic) Surgery
- Facial Trauma
- Cleft Lip And Palate
- Obstructive Sleep Apnea
2D & 3D IMAGING
2-dimensional imaging, such as routine dental and panoramic radiographs, have been mainstays of oral and maxillofacial surgical care. However, your surgeon may determine that for your care more advanced imaging may be needed. This includes hospital-based magnetic resonance imaging (MRI), computed tomography (CT), or an office-based cone beam CT (CBCT) scans.
CBCT scans are fast and convenient imaging modality that are excellent for dental implant planning, visualization of abnormal teeth, evaluation of the jaws and face, cleft palate assessment, diagnosis of dental caries (cavities), endodontic (root canal) diagnosis, and diagnosis of dental trauma. The imaging is usually completed in just a few minutes.
At our practice, we are pleased to offer CBCT imaging for the patients living in our communities.
The Carestream CS9600 system gives our oral and maxillofacial practice state-of-the-art technology to help Dr. Daisy Chemaly and Dr. Marco Magalhaes diagnose potential issues more accurately and provide treatment with unprecedented confidence. Unlike a traditional spiral CT scanner, this 3D system utilizes cone beam CT technology and provides precise, crystal-clear digital images while minimizing your exposure to radiation.
Our new 3D system enables us to perform a wider range of diagnoses and treatments in our office, helping to reduce multiple visits and outgoing referrals. The 3D scanner allows us to choose the field of view, or scanning area, that best suits your specific treatment needs. This helps to limit your radiation exposure because we are focusing specifically on your area of concern.
The Carestream CS9600 3D system brings the latest 3D technology to Dr. Daisy Chemaly & Associates, providing unmatched visualization of anatomical detail which aids in treatment planning and helps us to better explain the particulars of your case, as well as address any questions you may have. Drs. Daisy Chemaly and Marco Magalhaes can use this innovative technology to quickly and easily share 3D images of the area of concern with your referring doctor – allowing the doctors to collaborate on your care, improving your experience, and delivering a positive treatment outcome.
All About Wisdom Teeth
Scientists tell us that human jaws are gradually becoming smaller, as a result of evolution. This tendency to smaller jaw in modern man is the most probable cause of impacted wisdom teeth. Impacted means the tooth is stuck under gum and jaw bone and is unable to come into a useful, healthy position in the mouth. Teeth become impacted due to a lack of room in the jaws, or incorrect positioning. This is a common problem. The removal of impacted wisdom teeth is one of man’s most common surgical operations. Wisdom teeth develop during the adolescent years. If there is inadequate space, certain problems may arise.
1. Pressure may be created, causing pain in the jaw, ear and headache. This same pressure can cause damage to healthy, adjacent teeth.
2. Infection of the tissue around the wisdom tooth. This is called peritonitis, and is caused by food and bacteria which accumulates under gum tissue overlying impacted wisdom teeth. This can be quite painful, with possible development of severe infection.
3. Dental Crowding. Many experts are concerned that pressure from erupting wisdom teeth can cause crowding in adjacent teeth.
4. Cyst and Tumour Formation. Developing teeth normally have a sac around the crown. This disappears when the tooth grows into the mouth. If the tooth is impacted, the sac can grow and develop into a cyst or benign tumour. Rarely, malignant tumours have been seen in these sacs.
5. Malocclusion. Poorly positioned wisdom teeth can interfere with the fit between top and bottom teeth.
The Removal Of Impacted wisdom Teeth
While removal of impacted wisdom teeth is quite common, it does not mean the surgery is easy, or should be taken lightly. Wisdom teeth removal can be very simple or very complicated. The details of surgery are usually discussed at the pre-surgical consultation.
Impacted wisdom teeth are most frequently removed in the oral surgery clinic. Patients with very difficult surgery or coincident medical problems may have their surgery done in hospital. The decision as to where your surgery will best be done will be made by you and your oral surgeon.
Regardless of location, you will be kept completely comfortable during your surgery. I.V. sedation or general anaesthesia is most frequently used to maintain complete comfort during surgery. Local anaesthesia is generally used also. Simpler extraction procedures are frequently done with local anaesthesia (freezing) alone, or freezing and “laughing gas”.
Recovery Period. Most patients having impacted wisdom teeth removed will require some recovery time. The average varies from four to seven days following surgery. Simple extractions require less time. Difficult surgery may require more time.
Swelling and bruising are common after removal of impacted teeth. The swelling gener-ally peaks after two to three days.
It generally takes five to seven days to go away. This is a normal part of the healing mecha-nism. Anti-swelling medication is frequently given to reduce the amount and duration of post-surgical swelling.
What is an impacted tooth?
A tooth that is blocked by another tooth or dense bone and is therefore prevented from entering and assuming its normal place in the mouth is called an impaction.
What harm do impacted teeth do?
1. A cyst can form around the crown of the impacted tooth and cause destruction of surrounding bone and damage to other teeth and nerves in the area.
2. Whenever saliva can reach the impacted tooth, decay may occur and, since such cavities cannot be filled, severe toothache can result.
3. Bacteria in the saliva may cause infection around the crown of the impacted tooth. This infection may spread to the cheek, throat, or neck with pain and stiffness of the jaws.
4. A benign tumour may develop in the wall of a cyst surrounding the impacted tooth. This may require surgical treatment which is more complicated in order to correct. Unfortunately, impacted teeth can be “dormant” for years, but then cause problems and pain at an unexpected and inconvenient time. The removal of impacted teeth may therefore be a considered treatment and most surgeons recommend their removal even if they are not causing trouble now.
5. Your orthodontist may recommend preventative removal for space/crowding considerations or exposure of the tooth to bring it into the mouth.
Dental Extractions
The extraction of teeth may be required for any of the following reasons:
- Decayed or broken teeth which cannot be restored.
- Periodontal disease (pyorrhea) which has caused the teeth to become loose.
- Pathology associated with the tooth, such as cysts and tumors.
- Fracture of teeth due to facial trauma.
- Infection of the teeth or bone which cannot be treated by other methods.
- Poor positioning or crowding of teeth, including impacted wisdom teeth and extractions for orthodontic purposes.
The extraction of teeth is usually uncomplicated; however an incision may be required to assist in the complete removal of the root. In some cases, judicious bone removal to better expose the tooth maybe required. Sutures (stitches) may be placed at the extraction sites to control bleeding and to re-approximate the soft tissues. You will be told if you must return to have these removed.
In order to make you more comfortable during surgery, we have several techniques including local anesthesia, intravenous sedation and general anesthesia. These anesthetic options will be discussed with you at the time of your consultation.
During your initial examination, with the aid of appropriate radiographs, your surgeon will discuss the surgical treatment and anesthetic options. During this time, pre-operative instructions will be reviewed with you.
While recovery from extractions is generally uneventful, it would be prudent to limit physical activity for the first 24-48 hours post-operatively. If an intravenous or general anesthetic is to be used for your surgery, avoid intake of any food or liquids from the midnight prior to your surgery. Your surgeon will review your current medications with you. Some medications, such as blood pressure medicines or heart pills, may be taken with sips of water, while some need to be avoided. Additionally, if sedation or general anesthesia is being planned, you would need to be accompanied by a responsible adult.
Bone Grafting And Reconstruction
When an area of your body is missing bone, this deficient area is frequently called a “bony defect”. These defects may be as a result of:
• Trauma
• Tooth extractions or long-term tooth loss
• Cysts or tumor surgery
• Periodontal (gum) disease
A bone graft is a surgical procedure that replaces missing bone with material from the patient’s own body (autogenous) or with an artificial, synthetic or natural substitute (allograft). The graft not only replaces the bone, but can actually help your body to re-grow bone that has been lost. Depending on the anatomic region, a variety of augmentation techniques may be used. Your surgeon will determine your particular needs and will recommend the appropriate technique as well as any alternatives. If autogenous graft is recommended, appropriate sites and anesthetic options will also be reviewed at that time.
Sinus Augmentation (Sinus Lift)
A sinus lift of maxillary sinus floor augmentation is a surgical procedure which serves to increase the amount of bone in the posterior upper jaw. This procedure also involves raising the sinus floor and developing sufficient bone for the placement of dental implants. The maxillary sinuses are located behind your cheeks and above the upper teeth. These sinuses are empty, air-filled spaces. The roots of the natural teeth (upper arch) can extend into the maxillary sinuses. After a tooth extraction, the sinus tends to descend, and surrounding volume of bone is lost. Several techniques (direct and indirect) can be used to raise the sinus and facilitate the development of bone. Studies have shown that a sinus lift can greatly increase the success of implants.
Distraction Osteogenesis
This procedure involves treatment for selected deformities and defects of the jaw and skull. This advanced procedure allows an Oral and Maxillofacial Surgeon a safe and predictable approach to treating selected deformities. This procedure in most cases can be completed in our practice. More advanced cases are completed in the hospital. The surgery is conducted under anesthesia and is moderately invasive.
Dental Implants
If you are missing one or more teeth or are bothered by dentures or partials that slip, dental implants may be right for you! Besides the obvious cosmetic inconvenience of missing teeth, additional oral and general health problems may result when teeth are not replaced. Missing teeth can result in “tooth extrusion” or movement of another tooth into the empty space. Shifting or movement of adjacent teeth that occurs when tooth roots are not present may require additional orthodontic correction or treatment. Because of the misalignment that occurs due to shifting of teeth, the teeth may be more susceptible to decay and gum disease, possibly leading to additional tooth loss. Missing teeth can decrease chewing ability and may also affect speech.
If your upper or lower jaw is “edentulous” (all the teeth in that jaw are missing), “bone resorption” will occur over time in that jaw. The body “resorbs” the jawbone that used to surround the roots, causing the bone to “shrink”. This frequently causes problems for denture wearers because as the jawbone shrinks, dentures can become loose. When dental implants are placed, bone loss is often reduced or eliminated.
What is a Dental Implant?
Natural teeth are stable biting and chewing surfaces because the teeth roots are firmly anchored and supported by the surrounding jawbone. Dental implants function almost the same way. Implants are tooth root substitutes that look, feel and function much like the roots of natural teeth. Dental implants can replace a single missing tooth or several missing teeth.
Studies have shown dental implants to have a high rate of success, and can last for many years when cared for properly. The implant itself is a tiny metal cylinder that is surgically inserted in the jawbone. The material used for the dental implant is biocompatible, meaning it is well accepted by the body. Over time, the jawbone surrounding the implant grows into the implant surfaces and attaches to the implant, anchoring it firmly in place. This process of bone attachment is known as “osseointegration”.
A single tooth implant involves three separate parts: the implant root, the post that supports the artificial tooth (abutment) and the prosthetic tooth (crown or cap). The artificial tooth may be cemented onto the post or held in place with a tiny screw.
Dental implants can be used in people of all ages. However, you must be evaluated by your surgeon and restorative dentist to determine if you are a good candidate. Sometimes bone grafting is necessary prior to implant placement. With dental implants, you will rediscover the comfort and confidence to eat, speak, laugh and smile!
Guided Implant Surgery
Computer guided implant surgery is a revolutionary procedure involving the replacement of teeth with dental implants. This advanced virtual system allows our surgeons to determine the ideal sites for implant placement and expediates the restorative phase of treatment. Detailed planning is involved in this phase of treatment.
- CBCT scan which confirms the quantity and quality of the patient’s bone structure in 3D.
- Our surgeons are able to plan the surgery based on this information and simulate the implant positioning as well as the bone augmentation.
- A computer-generated surgical guide is ordered specific to the above information.
- Our surgeons are able to proceed with the surgery (typically under anesthesia for your comfort) delivering a more predictable and precise result.
Oral Pathology
Diseases of the oral and facial region may emanate from any of the structures and tissues of these regions such as bone, muscle, gum, fat and taste buds. While most are benign some may become malignant. Moreover, some of the “benign” lesions may behave in a destructive manner. Fortunately, early detection and treatment will, in most circumstances, cure the disease, or may mitigate the adverse effects.
As part of your physical examination, your dentist or physician would also examine your head and neck region, including the oral cavity. If there are any suspicious areas, you may be referred to an oral and maxillofacial surgeon, for biopsy and/or treatment. Depending on the nature of the disease, advanced imaging studies, such as MRI, CT scan, or other investigations may be necessary before treatment is offered.
TMJ (Temporomandibular Joint)
If a disorder exists with this joint, it can make eating, talking and even yawning painful. Temporomandibular joint (TMJ) disorders can be relatively minor or extremely debilitating. There may be many reasons for a TMJ disorder: clenching or grinding of the teeth, tightening jaw muscles, disease or injury can cause problems with your TM joint. These disorders can display a variety of symptoms including:
- Clicking or popping of the joints
- Tender or painful jaw muscles
- Difficulty or pain upon opening or closing the mouth
- Frequent headaches or neck aches
- Pain in the TM joint
- Ringing or buzzing sound in the ears
- Sensation of stuffiness, pressure blockage or pain in the ears
- Dizziness or lightheadedness
- Decreased jaw opening
The cause of TMJ dysfunction may involve the muscles of the joint, the bite or the joint itself.
TMJ Disorders can be caused by:
- Stress on the surrounding muscles
- Teeth clenching or grinding also known as bruxism
- Stress, poor posture or body alignment can cause the muscles surrounding the joint to tighten or spasm
- Abnormal jaw growth
- Missing teeth
- Diseases such as arthritis
The balance between the muscles and TM joint is an important one in preventing and treating TMJ disorders. If left untreated, muscles and joints that do not work well together may become trapped in a cycle of spasms and cause further injury to the joint, muscles and surrounding tissue.
Treatment of TMJ Disorders
There are many surgical and nonsurgical treatment options or a combination of treatments that can help restore normal function. In some cases, relief from discomfort can come from self-care techniques under the direction of your surgeon.
Corrective Jaw (Orthognathic) Surgery
The way your facial bones develop will affect your oral health, facial appearance and proportion. The position and size of your facial bones and teeth will determine how well you bite, chew and speak.
Any of the following symptoms may indicate a need for Corrective Jaw surgery:
- Difficulty chewing or biting food
- Difficulty swallowing
- Chronic jaw pain
- Excessive wearing of teeth
- Open bite (a space between upper and lower teeth when the mouth is closed)
- Overbite or under-bite
- Unbalanced facial appearance
- Facial injury or a defect from birth
While the correction of the above problems will obviously lead to improved function, it may also improve the facial esthetics. Treatment of a vast majority of these conditions would require a team approach and collaboration between an oral and maxillofacial surgeon as well as other professionals such as orthodontists, prosthodontists, family dentists, and others.
During your initial consultation, your surgeon, after examination, will thoroughly discuss your condition as well as treatment options and timeline of your care.
Facial Trauma
Facial Trauma can result from motor vehicle accidents, accidental falls, sports injuries, interpersonal violence and work-related injuries. Types of facial injuries can range from injuries of teeth to extremely severe injuries of the skin and bones of the face. Typically, facial injuries can be classified as soft tissue injuries (skin and gums), bony injuries (fractures), or injuries to special regions (such as the eyes, facial nerves or the salivary glands).
Oral and Maxillofacial Surgeons are specially trained and highly skilled in treating facial trauma such as:
• Intraoral lacerations
• Fractured Teeth
• Fractured Facial bones
• Fractured Jaws
• Lip Lacerations
• Facial Lacerations
• Teeth that have been knocked out
One of the most common types of serious injury to the face occurs when bones are broken. Fractures can involve the lower jaw, upper jaw, palate, cheekbones, eye socket, and combinations of these bones. These injuries can affect the ability to breathe, speak, chew and swallow. Treatment frequently requires hospitalization but less serious injuries can be treated in our office.
Of course, not all facial injuries are extensive. The thing you should remember, though, is that they are all complex. Even in the case of a moderately cut lip, the expertise of the oral surgeon is indispensable. If sutures are needed, placement must be precise to bring about the desired cosmetic result. So a good rule of thumb is that you shouldn’t take any facial injury lightly.
Some of the signs and symptoms of facial fractures are:
• Pain
• Numbness of the lip, cheek, tongue, nose
• Inability to open the mouth
• Change in the bite
• Visible step-off between teeth
• Deep laceration over bone
• Bleeding from the mouth or nose
Soft Tissue Injuries of the Face
When soft tissue injures, such as lacerations, occur on the face, they are repaired by “suturing”. In addition to the obvious concern of providing a repair which yields the best cosmetic result possible, care is taken to inspect for injuries to structures such as facial nerves, salivary glands and salivary ducts. Your doctor is a well-trained Oral and Maxillofacial surgeon and is proficient at diagnosing and treating facial lacerations.
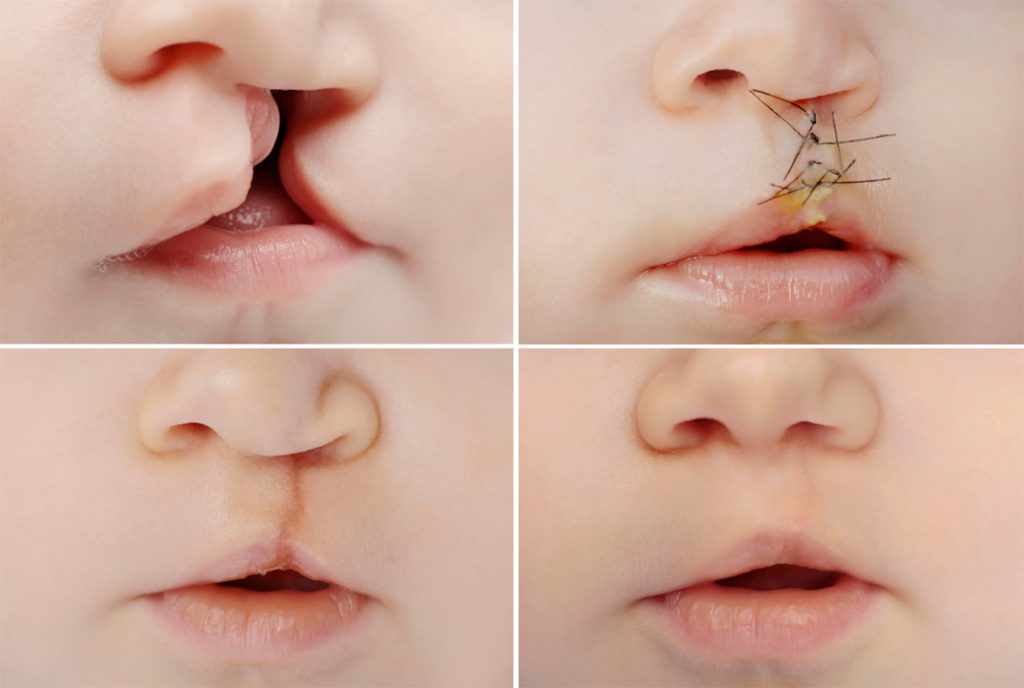
Cleft Lip And Palate
During early pregnancy, separate areas of the face develop individually and then join together, including the left and right sides of the roof of the mouth and lips. However, if some parts do not join properly, such as the palate (roof of your mouth) or upper lip, the result is a cleft. If the separation occurs in the upper lip, the child is said to have a cleft lip and if it is in the palate, it is called cleft palate.
Oral and maxillofacial surgeons are involved in treating these patients with a group of other health professional experts to provide the best treatment for this condition.
Obstructive Sleep Apnea
People with obstructive sleep apnea (OSA) have disrupted sleep and low blood oxygen levels. When obstructive sleep apnea occurs, the tongue is sucked against the back of the throat, which blocks the upper airway and airflow stops. When the oxygen level in the brain becomes low enough, the sleeper partially awakens, the obstruction in the throat clears, and the flow of air starts again, usually with a loud gasp. Additionally, these individuals suffer from excessive daytime sleepiness, depression, and loss of concentration.
The first step in treatment resides in recognition of the symptoms and seeking appropriate consultation. Oral and maxillofacial surgeons offer consultation and treatment options.